How did they celebrate the fourth of July 4th at Fort Amanda in 1813; short answer, they didn't. and entries from Ensign William Schillinger's journal entries from June 27 - July tells us why.
First of all, If you had been at Fort Amanda 212 years ago on July 4th, when you walked through the southwest gate, the first thing you probably would have noticed is the smell. Today the area around the monument today looks like a well groomed lawn but in 1813 it's doubtful there was much if any grass inside the fort walls. The foot, animal and wagon traffic would likely have reduced the grounds to a muddy mess particularly on rainy days. Despite efforts to keep the grounds clean, the mud, and stench eminating from the animal pens and butchering areas to southeast of the fort as well as from the latrines would have made your visit very unpleasant.
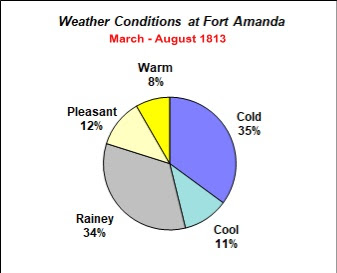
Adding to the misery of life at Fort Amanda was the everchanging Ohio weather. During the time Schillinger's company was stationed there, (March through August 1813), 80 percent of the time, the weather was either cold, cool or rainey. Such was the case at the end of June 1813 when the first cases of the dreaded measles appeared at the fort .
Measles can affect the eyes causing them to become red and swollen creating an extreme sensitivity to light. In 1812 the common treatment was a potion called “eye water.” In the field, soldiers made eye water by taking the scrapings from a Turmeric root, mixing it with water and dropping it into the eyes several times a day. To help ease the cough that goes along with the ailment, they mixed water with lemon and honey which helped relax airways, loosen mucus. Seriously ill soldiers at Amanda were placed in darkened cabins to protect their eyes from the sunlight..
The following are Schillinger's journal during the measels outbreat at the fort. They are shown exactly as written. No spelling or grammar errors have been corrected.
Sunday June 27 - Clear and warm, nothing particular xcept, one of our Men who was sick started to go home, (Peter Westerfield, a private in our company).
Monday June the 28th 1813 - Warm & Dry, Some of our men sick with the meazels, nothing particular to Day
Schillinger's Sense of Humor?
That afternoon Schillinger and Sgt. Bradbury went into the woods looking for some turmeric roots and honey. They found the roots and while they were able to find a source for some honey, apparently it wasn’t as easy to gather.
The journal entry reads “found A Bee Tree or swarm of bees in a tree.” In today’s vernacular what he may have been saying was “we found a swarm of bees in a tree.
The two men brought their root scrapings and their honey back to the fort and made up a batch of eye water for the men in the company.
Tuesday the 29th - Continued warm, Order from General wingate to the Captn & myself to attend A court martial as members, immediately at St. Marys - took A walk out with Sergant Bradbury this afternoon to get some root to make Eye water, Got some, found A Bee Tree or swarm of bees in a tree.- A number of our men sickening. for the meazels, The Cap,t complaining A little this evening, 1st sergt quite unwell
Wednesday the 30th - Started early this morning in company with Capt Hosbrook for St. Marys, to attend court martial arrivd at St. Marys formed our Court etc. as follows.
Thursday the 1st July 1813 - Heavy Showers this morning 10 oclock A.M. Left St. Mary for fort Amanda. arrivd at 3 P.M. found A number of our Company sick some with the meazels.
Friday the 2nd - Rainy, Captn Sick the meazelss out on A number of our company & others sickening, Major Miligin & Major Ludwick went to St Marys. Clouds Broke away in the evening.
Saturday the 3rd - This morning Clear & pleasant, we got A good Mess of fish out of the fish Pot, Thunder Showers in the afternoon 4 men from fort Jennings arrivd, on their way homeSunday the 4th July 1813
Our men many of them sick prevented us from Celebrating the Day in the usual way, Capt G. R. Benagh went to Fort St. Mary to join in Celebrating the memorable Day. This being Cool & pleasant with A fine Breeze of wind at about, W. made our situation quite comfortable to what it had been for some days past
Monday the 5th - This morning Cool & Pleasant Our men some of them on the mend & some sickening for the meazels, 11 A.M. Mr. Kerchard arrivd at fort from the rappids Informed us that the coast was clear of the enemy. that there was none of them about fort meigs, Dr. Lewis came to fort with Mr. Benagh.
The Outbreak Ends
The only recorded death was that of a young soldier named Charles Murry. He died the first of June 13 and is buried inside the fenced area near the ravine. What he died of remains a mystery but the question will always remain; "Was he the first casualty of the Measels Outbreak of 1813?"